
AFWG shall not bear any responsibility for any content on such sites. Any link to a third-party site does not constitute an endorsement of the third party, their site or services. AFWG also makes no warranties as to the content of such sites.
Would you like to continue?
Dr Methee Chayakulkeeree
Associate Professor
Division of Infectious Diseases and Tropical Medicine
Faculty of Medicine Siriraj Hospital
Mahidol University
Bangkok, Thailand
Clinical presentation
A 65-year-old man presented to the hospital with prolonged fever of 3 months. His underlying medical conditions included type 2 diabetes (managed with premix insulin twice a day), hypertension, coronary heart disease, dyslipidemia and cervical cord tumor with paraplegia. He complained of weight loss of 25 kg within the last 6 months. His test for HIV was negative.
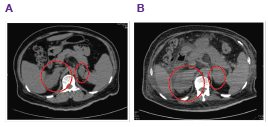
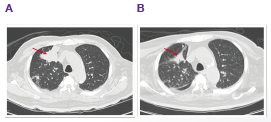
Ultrasonography of the abdomen showed an oval-shaped, hypoechoic, right suprarenal mass (3.9×2.4 cm). CT scan of the abdomen showed lipid-poor masses at both adrenal glands with central necrosis (Figure 1A). There was no internal calcification or adjacent organ invasion. CT scan of his chest revealed enhancing mass at right upper lobe (RUL) with central necrosis, internal calcification and speculate border (Figure 2A). There was also multiple heterogeneous enhancing masses at the RUL intrapulmonary nodules and right middle lobe (RML) with interlobular septal thickening. The patient was suspected to have bronchogenic carcinoma with intrapulmonary, lymphangitic and adrenal metastases.
The patient developed hypotension, adrenal insufficiency and was tested positive for tuberculosis in the bronchoalveolar lavage fluid. He was diagnosed with disseminated tuberculosis and commenced treatment with isoniazid, rifampicin, ethambutol and pyrazinamide until the third week when anti-tuberculosis therapy was stopped due to elevated liver enzymes. He experienced adrenal crisis and was treated with hydrocortisone 100 mg intravenous (IV) push followed by 200 mg IV drip in 24 hours. He resumed anti-tuberculosis treatment (isoniazid, rifampicin and ethambutol) 11 days later.
He was admitted to the hospital again 2 months later for prolonged fever and low blood pressure (87/59 mmHg), complaining of nausea, vomiting and weight loss. He was treated with hydrocortisone 100 mg/day and meropenem 1g IV every 8 hours. Lung CT scan showed decreased mass in the RUL and diffuse centrilobular nodules at RUL and RML (Figure 2B). Abdominal CT scan showed enlarged bilateral adrenals (Figure 1B). Brain CT scan showed multiple ring enhancing hypodensity lesions at right occipital region, right temporal, left side pons and right cerebellum. Culture of the tissue biopsy at the right adrenal mass grew Histoplasma capsulatum. The patient was diagnosed with disseminated histoplasmosis. He was treated with amphotericin B at 0.7 mg/kg/day for 4 weeks then maintained with itraconazole (600 mg/day for 3 days followed by 400 mg/day for 12 months). The patient continued to receive IV hydrocortisone and fluid support throughout his antifungal treatment.
Discussion
This case demonstrated the management of a patient with disseminated tuberculosis and histoplasmosis with adrenal insufficiency. Tuberculosis and histoplasmosis have similar symptoms.1 Although these pathologies share certain similarities, there are clinical and laboratory differences. Differential diagnosis is important especially in Asian countries where both diseases are endemic. Disseminated forms of both diseases are rare but may occur in immunocompromised patients or patients with chronic medical conditions.1
Chest pain, cough and abnormal chest radiograph results are commonly associated with tuberculosis.1 Conversely, abnormal imagery of the abdomen, in particular the enlargement of bilateral adrenal glands are more frequent in patients with histoplasmosis.1,2 Differential diagnoses for both diseases can be further confirmed by culture results and PCR assays. They should be systematically tested without delay as a great number of patients with adrenal histoplasmosis may develop life-threatening adrenal insufficiency if untreated.2
Clinical pearls
Highlights of the Medical Mycology Training Network Conference, December 1–3, 2017, Ho Chi Minh City, Vietnam
References