

AFWG shall not bear any responsibility for any content on such sites. Any link to a third-party site does not constitute an endorsement of the third party, their site or services. AFWG also makes no warranties as to the content of such sites.
Would you like to continue?
![]()
Tan BH, Chakrabarti A, Patel A, Chua MMM, Sun PL, Liu Z, Rotjanapan P, Li R, Wahyuningsih R, Chayakulkeeree M, Chen YC; Asia Fungal Working Group (AFWG).
Int J Infect Dis 2020;95:271-280
HIGHLIGHTS
|
Clinicians in Asian countries face significant challenges in diagnosing and treating IFDs with limited resources. The AFWG conducted the gap-analysis survey to identify the gaps and needs for improving the outcomes of IFD in this region.
“We suspect that physicians in Asia face multiple challenges in the care of patients with IFD, but there are no objective data on the nature and extent of these challenges”
The AFWG conducted a 22-item, web-based survey on management practices for IFD among clinicians in China, India, Indonesia, Philippines, Singapore, Taiwan and Thailand. The survey was open to all clinicians managing IFDs, in particular doctors from the fields of infectious disease, critical care, transplant medicine, hematology and oncology.

“This is the first multinational clinicians’ survey on mycology practice patterns”
The survey identified inadequacies in medical mycology training, non-culture-based diagnostics, access to antifungal drugs, and local guidelines as the major gaps in the management of IFDs in Asian countries.
Among 292 respondents from 7 countries: India (n=109), the Philippines (74), China (34), Taiwan (27), Indonesia (17), Singapore (17) and Thailand (14), only 37% of respondents had received formal training in medical mycology. Despite the view that training in medical mycology had been suboptimal, only a minority of non-ID respondents referred patients with IFDs to ID physicians.
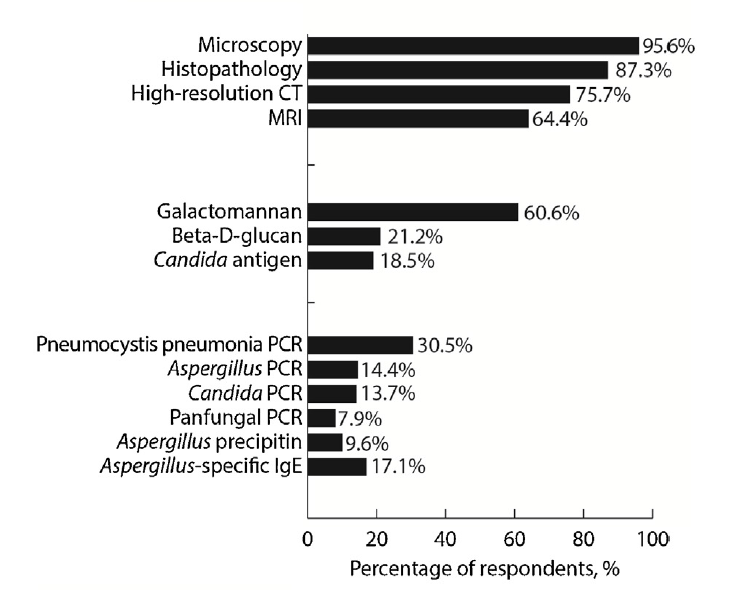
The majority of respondents had access to direct microscopy (96%) and histopathology (87%), while galactomannan and azole levels were available to 60% and 25% of respondents, respectively (Figure 1). The findings suggested that clinicians were sending their specimens outside their hospital for assays such as galactomannan and azole level monitoring.
Figure 1. Accessibility of laboratory diagnostics for the management of patients with fungal infections
The majority (84%) used clinical parameters for treatment response monitoring, and 78% of respondents stated that they followed the Infectious Diseases Society of America (IDSA) guidelines on the management of IFDs. Where febrile neutropenia was concerned, 74% of respondents used the empirical approach. 80% could not use preferred antifungals because of cost. Only 30% had an antifungal stewardship program in their hospital.
The majority (70%) of 292 respondents agreed that country-specific training courses, improvement of laboratory diagnostic methods in hospitals and development of institute-based or country guidelines are top strategies to improve the management of IFDs.
The authors recommended referring patients who are suspected or confirmed to have IFD to an ID physician. Where ID physicians are in short supply, involving an ID physician in the development of an intra-hospital guide on IFD management was recommended.
Some efforts have been carried out to fulfil these needs. For example, the AFWG has conducted courses on medical mycology in Indonesia, Malaysia, the Philippines, Singapore, Taiwan, Thailand and Vietnam in the last 9 years. Laboratory attachments sponsored by the AFWG have also been organized to enhance the skills of young microbiologists from less privileged areas. However, there are still huge unmet needs – support from governments and international agencies is needed to fill these gaps.