
AFWG shall not bear any responsibility for any content on such sites. Any link to a third-party site does not constitute an endorsement of the third party, their site or services. AFWG also makes no warranties as to the content of such sites.
Would you like to continue?
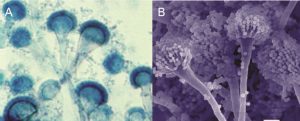
Aspergillus, of which A. fumigatus is the most commonly isolated species, is an important etiology of life-threatening fungal infections in the immunocompromised population, including those with prolonged neutropenia, transplant recipients and HIV-afflicted patients with advanced disease. As cited in the 2008 Infectious Diseases Society of America (IDSA) treatment guidelines, aspergillosis causes patient afflictions that are classically defined as invasive (respiratory, central nervous system and other organs), saprophytic (otomycosis and pulmonary aspergilloma) or allergic (sinusitis and allergic bronchopulmonary aspergillosis [ABPA]).1
Proven aspergillosis requires histopathological evidence of infection and a positive culture of a specimen from a normally sterile site. Probable aspergillosis requires fulfillment of criteria within 3 categories: host factors, clinical manifestations (symptoms, signs and radiological features), and microbiological evidence. Therefore, proven or probable infection requires the recovery of Aspergillus. However, there are 2 exceptions cited in the IDSA guidelines.1 The first exception includes the fairly frequent occurrence of histopathological demonstration of hyphae consistent with Aspergillus species in patients with negative culture results. The other exception is the use of a surrogate non–culture-based method (ie, a positive galactomannan assay or (1-3)-β-D-glucan assay result and radiologically compatible CT findings) in an immunocompromised host with clinical findings of infection that constitute the definition of probable invasive aspergillosis.