
AFWG shall not bear any responsibility for any content on such sites. Any link to a third-party site does not constitute an endorsement of the third party, their site or services. AFWG also makes no warranties as to the content of such sites.
Would you like to continue?
Professor Yee-Chun Chen
Professor of Medicine
National Taiwan University Hospital and College of Medicine; and
Investigator, National Institute of Infectious Diseases and Vaccinology
National Health Research Institutes
Taiwan
Fungal pathogens pose a significant threat to public health, food biosecurity and biodiversity. Despite this, they are largely ignored by the public, the press and funding bodies. From a public health perspective, there remains relatively little global recognition that over 300 million people suffer from serious fungal-related diseases, or that fungi are responsible for an estimated 1.6 million deaths each year – a higher mortality rate than that of malaria.1
Cryptococcosis
Around 21–36% of cryptococcosis cases occur in patients with cirrhosis, making it the most common host factor associated with these infections in HIV-uninfected patients.2-4 Furthermore, in a recent multivariate analysis, cirrhosis was 1 of 2 factors (along with cerebrospinal fluid antigen titer) shown to be an independent predictor of mortality.4 The minimum inhibitory concentration (MIC) of different antifungal agents, particularly fluconazole, may vary according to genotype; hence it is important to determine MICs for clinical isolates.
Candidemia
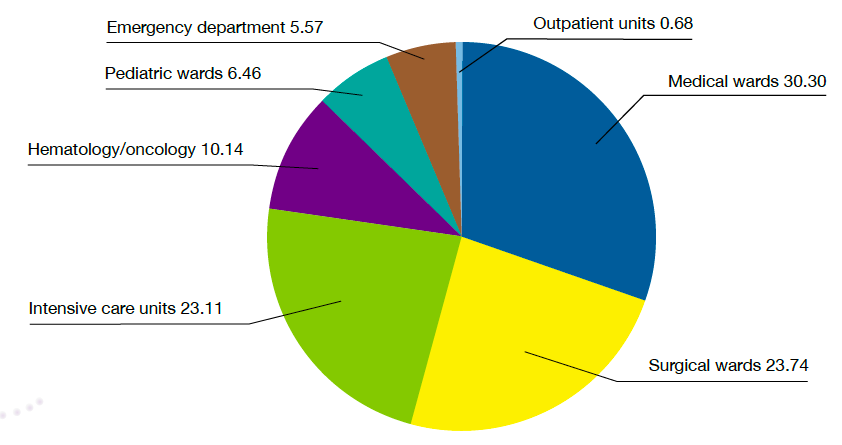
A recent laboratory-based surveillance study conducted in 25 hospitals across Asia demonstrated that candidemia is common across the region, with an overall incidence of more than 1 episode per 1,000 discharges, and a wide distribution across services (Figure).5 Candida tropicalis was the most frequently isolated non-albicans species, particularly in tropical countries.5,6 Risk factors for candidemia include age, moderate-to-severe renal diseases, leukemia, lymphoma, gastrointestinal malignancies, metastatic solid tumors and chronic pulmonary diseases.7
Figure. Distribution of patients with candidemia by hospital service (numbers denote percentages)5
In a pan-Asian study, reduced susceptibility to fluconazole was common in non-albicans Candida species, suggesting that echinocandins should be the antifungal of choice in clinically unstable or high-risk patients with documented candidemia.6 International guidelines recommend echinocandins as initial therapy for candidemia in most cases.8,9
Aspergillosis
In a recent study conducted in 5 Asian countries, Aspergillus species was the most common etiology of microbiologically confirmed cases with proven/probable invasive mold infection (71.6%) – largely due to A. fumigatus and A. flavus.10 The most frequently observed host factor was prolonged steroid use (39.4%) and the most common underlying condition was diabetes (30.9%).10
Azole resistance in A. fumigatus is an emerging global health problem, including in Asia.11-13 This could affect the current primary treatment recommendation, which is based around voriconazole monotherapiy.14 Alternative treatment strategies, including azole-echinocandin combinations or liposomal amphotericin B, may be necessary in areas with environmental resistance rates of ≥10%.15
Highlights of the Medical Mycology Training Network Conference, August 5–6, 2017, Kuala Lumpur, Malaysia.
References